Chronic neck pain might start to construct slowly over time. Neck pain is persistent if it lasts longer than three months. The pain may come and go, or be worse with some specific movements. The pain might only affect your neck, or it can move for your arms, back, or shoulders. You might also have pain that begins in other body part and moves to your neck. You may additionally have neck pain for years. Some types of neck pain can become permanent.
Common causes of chronic neck pain
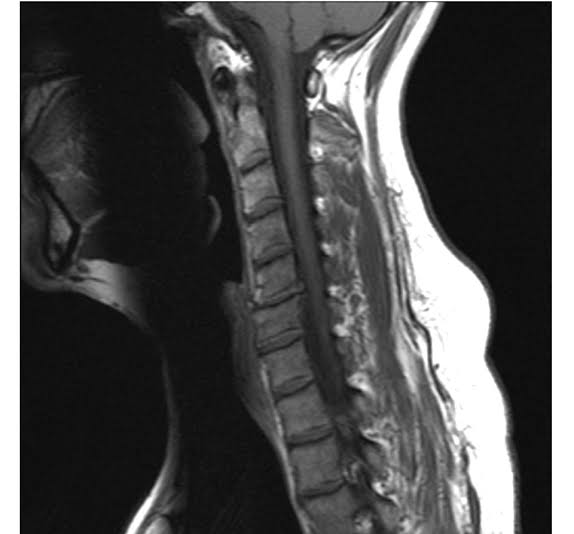
When neck pain lasts or maintains coming returned over duration of numerous months, its miles typically because of spinal degeneration from wear-and-tear over time (also referred to as cervical spondylosis). Disc related chronic neck pain causes are;
Cervical degenerative disc disease
All discs step by step lose hydration and the ability to cushion the spine’s vertebrae over time. If a disc degenerates enough, for a few people it is able to result in pain in diverse ways, along with a herniated disc, pinched nerve, or changes in the facet joints that can reason osteoarthritis.
Cervical osteoarthritis
When the cartilage in a cervical facet joint wears down enough, it can lead to cervical osteoarthritis. Cervical osteoarthritis is one of the most commonplace chronic neck pain causes.
Cervical herniated disc
When an intervertebral disc’s which is protecting outer layer (annulus fibrosus) in part or absolutely tears, a number of the jelly-like inner layer (nucleus pulpous) can also leak and reason inflammation and pain.
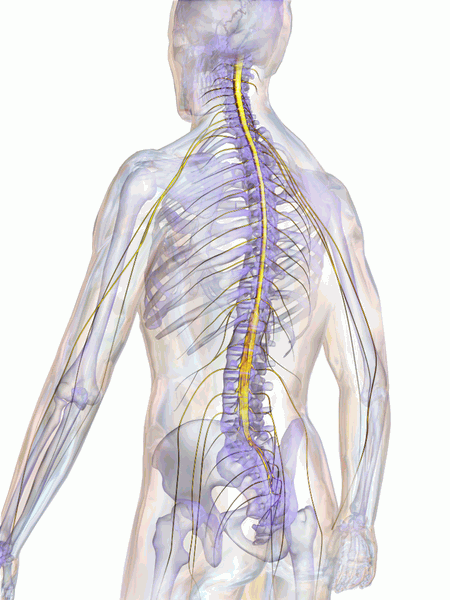
As spinal degeneration progresses, there is an increased chance for a narrowing of the foramen (cervical foraminal stenosis) and/or the spinal canal (cervical central stenosis). If the nerve root and/or spinal cord turn into impinged, pain, tingling, numbness, and/or weakness can also radiate into the fingers or legs.
Other causes of chronic neck pain
Other chronic neck pain causes could include;
- Emotional stress and anxiety
- Bad sleeping position
- Infection
- Myofascial pain syndrome
- Fibromyalgia
- Spinal tumor
- Spondylolisthesis
- A fraction of a neck bone that results in nerve damage
- A condition that affects neck to arm nerves, which may include thoracic outlet syndrome or brachial neuritis
- Inflammation from a medical condition such as rheumatoid arthritis, polymyalgia rheumatica, or rotator cuff tendinitis
Risk factors for developing chronic neck pain
Many exclusive risk factors for chronic neck pain causes had been suggested within the medical literature, such as:
- Reduced neck strength
- Previous neck problems
- Poor posture
- Smoking
- Labor-in depth occupation
- Female sex
- Feelings of low support from work, family, or friends
For further information call us on 815.412.6166