Orthopedic injury is a severe trauma to part of the musculoskeletal system, and often results due to sudden accident requiring immediate medical attention. While not all orthopedic injury is life-threatening, it is life altering. Therefore, you should choose doctor wisely.
Symptoms of orthopedic injury
Trauma to the bones and soft tissues that fall under orthopedic injury may be come by several possible symptoms, depending on which part of the body is affected. The most common symptoms of a broken body part or limb may include:
- Swelling
- Tenderness
- Bleeding, but only occurs if the break in the bone damages the skin
- Major bruising
- Inability or difficulty to move the affected part without pain
- Bone sticking out at an abnormal angle
- Bone sticking out of the skin
- Numbness
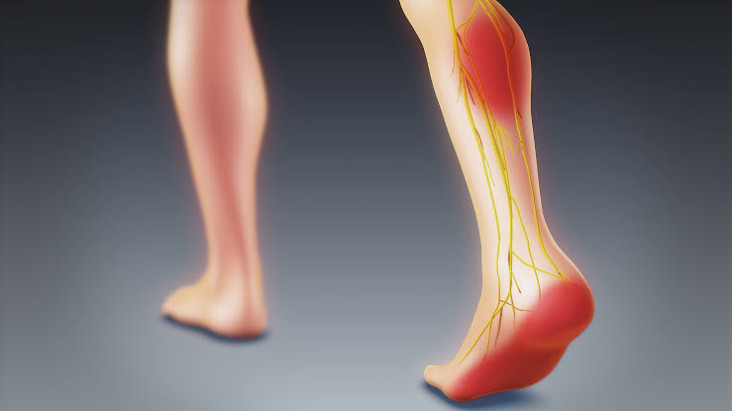
- A needles sensation if nerves has injured
- Helplessness to lifting or rotating the injured part
- Inability to put any weight if leg is injured
- Severe pain when breathing in (if ribs are broken)
- Shallow breathing
- A grinding, snapping or cracking noise is heard at the time of the fall or accident
Treatments for orthopedic injuries
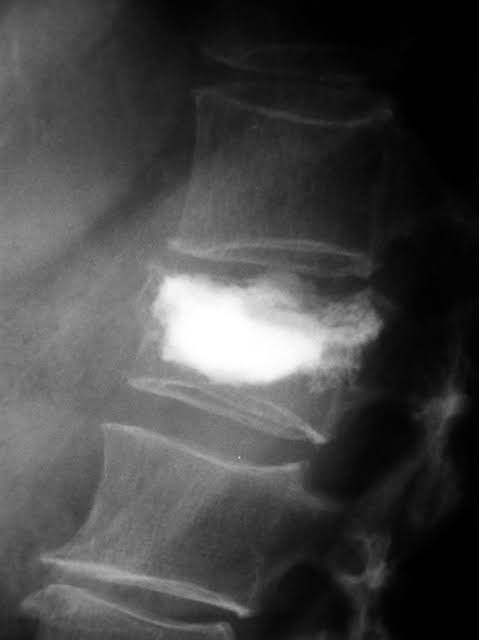
Orthopedic injury uses both surgical and non-surgical techniques to treat the affected bones and soft tissues depending on the severity of the condition. Minor dislocations and fractures of specific bones such as the clavicle, scapula and humerus can be treated with non-surgical measures through an external fixation method. This means that some orthopedic devices such as braces, casts, and splints are placed outside the body to keep the injured part stable or fixed during the recovery period.
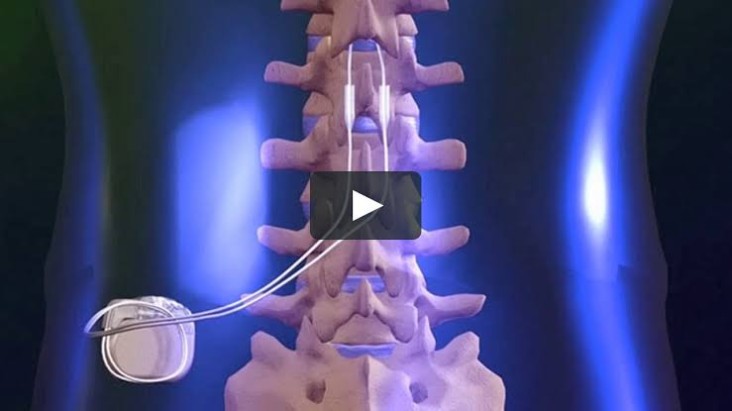
On the other hand surgical means for orthopedic injury, include:
- Minimally invasive surgery
- Conventional surgery
- Internal fixation method, which refers normally to surgically installing orthopedic devices on the bone itself
The following procedures are secured for more severe orthopedic injuries and might be done either conventionally or through minimally invasive techniques.
- Bone grafting and bone/joint transplantation
- Bone-forming
- Limb lengthening
- Lower limb reconstruction, such as hip and knee joint replacements
- Upper extremity reconstruction
- Soft tissue repair
How long does orthopedic injury take to heal?
Orthopedic injury is usually followed by a long recovery period, depending on the severity. The shortest recovery period is three weeks for minor injuries. Wrist, arm injuries, fractured collarbone take 6 to 8 weeks to heal. There are also some cases in which the bone fails to heal, results in permanent injury. Among all types of orthopedic injuries, broken hip has the longest recovery period. For many individuals it gets difficult to regain their original condition after suffering a fracture in the hip bone.
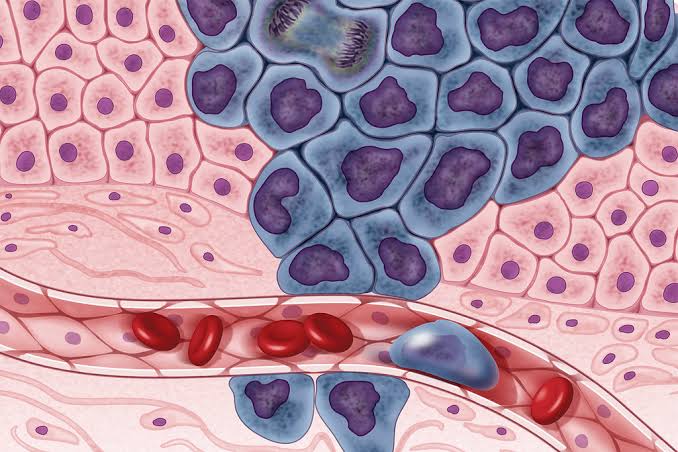
Pain management institute is helping people to cure acute and chronic long term pain to resume a normal life style. PMI has provided many treatments like stem cell therapy and many others.
For more details call on 815.412.6166